In North America, women under 50 represent 18% of breast cancer diagnoses.¹
Younger women² are more likely to be diagnosed later and more likely to develop aggressive forms of breast cancer, which leads to poorer outcomes.³ Earlier detection is needed now.
1 in 8 women will be diagnosed with breast cancer during her lifetime.
It is estimated that 316,450 women in North America will be diagnosed with breast cancer in 2022.³ ⁴ About 57,000 of those will be women under 50.
In Canada, screening recommendations are for women 50-74.⁵ There is no recommended screening for women under 50 of average risk.
When women have extremely dense breast tissue, more cancers are missed than are diagnosed with screening mammography.
Facts to know
Breast cancer research is advancing rapidly. Young women’s breast cancer is an area where new knowledge is starting to build and changing views of the characteristics of the disease in different age groups. Due to the poorer outcomes for younger women and lack of screening in this age group, expanding knowledge is key to earlier detection and better outcomes.
- Breast cancer affects women of all ages.
Most breast cancers occur in women 50 and older. While it’s less common for young women to develop breast cancer, it does happen. In fact, in North America, 18% of breast cancer diagnoses are women under 50.

- Most breast cancers are not associated with a genetic risk.
Breast cancer in young women has a higher probability of having a known genetic risk factor. For this reason, many guidelines recommend having a risk assessment around age 30. There are many online tools that can be used to assess individual risk of developing breast cancer.⁶ However most young women that develop breast cancer do not have a known genetic risk factor. This increases the need for women to be knowledgeable and pro-active regarding their breast health.

- Most breast cancers are not associated with a family history of breast cancer.
Most women diagnosed with breast cancer have no known family history of this disease. Despite this, a strong family history of breast cancer is still an important risk factor and is included in risk assessments.
< Only about 5–10% of breast cancers are believed to be hereditary, meaning they’re caused by abnormal changes (or mutations) in certain genes passed from parent to child. > The American Cancer Society

- Breast cancer has many sub-types, with young women having an increased probability of developing more aggressive sub-types.
There are several types of breast cancer and some are more common among younger women. Black women have a higher chance of developing breast cancer, and more aggressive cancer, before the age of 40 than other races/ethnicities.⁷
Types of breast cancer
- It is challenging to detect breast cancer in younger women.
Current screening guidelines in Canada recommend women between the ages of 50 and 74 receive screening mammography every two years. There is debate regarding if younger women should be included in regular mammography screening. This is based on many reasons, but the main principle is the balance of the benefits of regular mammography screening with the risks. Younger women are more likely to have dense breast tissue, which leads to a decrease in the ability of mammography to detect the presence of cancer.⁸ Inclusion of other imaging technologies such as ultrasound or MRI increases the probability of false positives, resulting in more procedures. There are many online tools that can be used to assess individual risk of developing breast cancer. Women at high risk may be recommended to receive screening imaging beginning at younger ages, depending on provincial guidelines.⁹
Roughly half of all women have dense or very dense breast tissue – a characteristic that’s more common among premenopausal (younger) women. Women with dense breast tissue have a higher risk of developing breast cancer than women less dense breast tissue.
-
Breast Cancer affects women of all ages.
Most breast cancers occur in women 50 and older. While it’s less common for young women to develop breast cancer, it does happen. In fact, in North America, 18% of breast cancer diagnoses are women under 50.
-
Most breast cancers are not associated with a genetic risk.
Breast cancer in young women has a higher probability of having a known genetic risk factor. For this reason, many guidelines recommend having a risk assessment around age 30. However most young women that develop breast cancer do not have a known genetic risk factor. This increases the need for women to be knowledgeable and pro-active regarding their breast health.
-
Most breast cancers are not associated with a family history of breast cancer.
Most women diagnosed with breast cancer have no known family history of this disease. Despite this, a strong family history of breast cancer is still an important risk factor and is included in risk assessments.
< Only about 5–10% of breast cancers are believed to be hereditary, meaning they’re caused by abnormal changes (or mutations) in certain genes passed from parent to child. > The American Cancer Society
-
Breast cancer has many sub-types, with young women having an increased probability of developing more aggressive sub-types.
There are several types of breast cancer and some are more common among younger women.
Types of breast cancer >
-
It is challenging to detect breast cancer in younger women.
Current screening guidelines in Canada recommend women between the ages of 50 and 74 receive screening mammography every two years. There is debate regarding if younger women should be included in regular mammography screening. This is based on many reasons, but the main principle is the balance of the benefits of regular mammography screening with the risks. Younger women are more likely to have dense breast tissue, which leads to a decrease in the ability of mammography to detect the presence of cancer.⁷ Inclusion of other imaging technologies such as ultrasound or MRI increases the probability of false positives, resulting in more procedures. There are many online tools that can be used to assess individual risk of developing breast cancer.⁸ Women at high risk may be recommended to receive screening imaging beginning at younger ages, depending on provincial guidelines.⁹
Roughly half of all women have dense or very dense breast tissue – a characteristic that’s more common among premenopausal (younger) women. Women with dense breast tissue have a higher risk of developing breast cancer than women less dense breast tissue.
< Dense breasts also make a mammogram harder to read. On a mammogram, fatty tissue looks dark, while dense tissue looks white, like tumours, so it can hide a tumour. > Canadian Cancer Society
Syantra DX™ Breast Cancer is a blood test for breast cancer detection that’s easy, convenient and accurate.
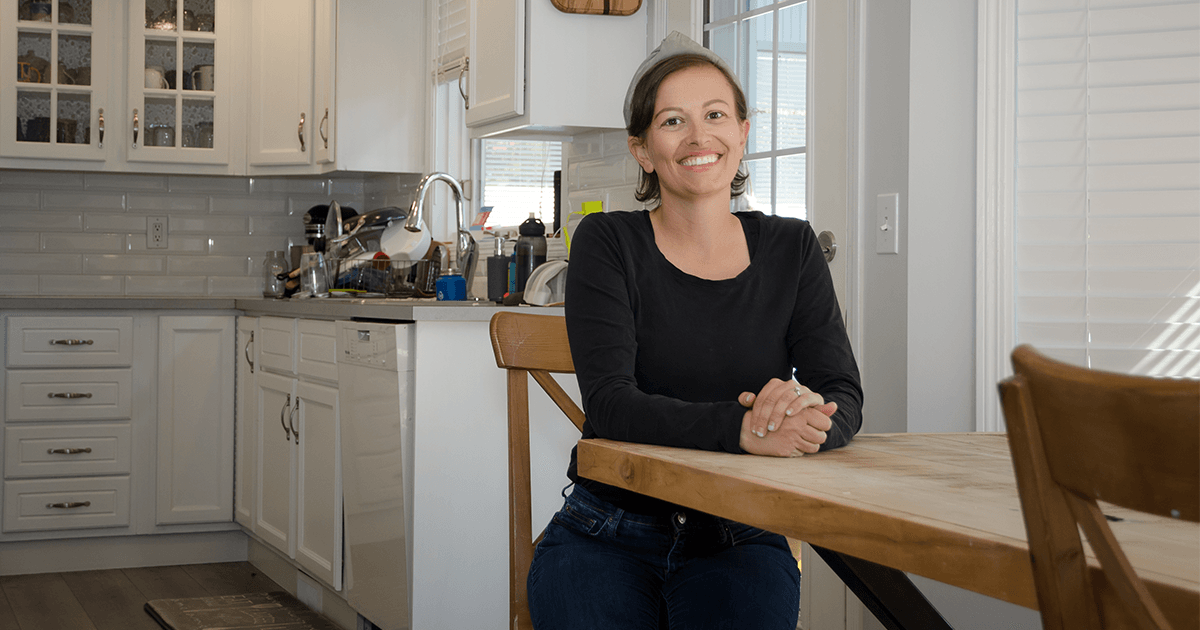
Voices from the 18%

Risk factors to know
< A risk factor is something that increases the risk of developing cancer. It could be a behaviour, substance or condition. Most cancers are the result of many risk factors. But sometimes breast cancer develops in women who don’t have any of the risk factors... >
Oral contraceptives
Oral contraceptives that contain both estrogen and progesterone can slightly increase the risk for breast cancer.
Reproductive history
Women who are older than 30 when they give birth to their first child have a higher risk of breast cancer.
Early menstruation
Starting your period early (11 and under) means that your cells are exposed to estrogen and other hormones for longer, which can increase the risk of breast cancer.
Lifestyle factors
Body mass, exercise and alcohol consumption all have a documented impact on breast cancer risk. Studies show that taking action on lifestyle risk factors can lower your risk of breast cancer.
Types and presentations of breast cancer
Invasive breast cancer is when malignant cells have broken through the duct or lobular lining, spreading into the adjacent breast tissue.
-
Invasive ductal carcinoma
Breast cancer that starts in the milk ducts, the tubes that carry milk from the lobules to the nipple. It’s the most common type of breast cancer.
-
Invasive lobular carcinoma
This breast cancer starts in the glands in the breast that produce milk (called the lobules). It’s the second most common type of breast cancer.
-
Triple-negative breast cancer
The name refers to the fact that the cancer cells don’t have the usual estrogen or progesterone receptors and make little or none of the protein called HER2. This type of cancer tends to be aggressive, has fewer treatment options, and leads to poorer outcomes. Triple Negative breast cancers are more common in women younger than age 40, who are Black, or who have a BRCA1 mutation.
-
Inflammatory breast cancer
A rare and aggressive form of invasive breast cancer that develops when cancer cells block the lymph vessels in the skin of the breast, causing the breast to appear red and swollen. Typically, as already spread to the lymph nodes or other organs on diagnosis. Inflammatory breast cancer occurs most often in young women and Black women.
-
Metastatic breast cancer
Also called stage IV breast cancer, is invasive breast cancer that has spread (metastasized) to parts of the body away from the breast, such as the bones, liver, lungs, or brain.
-
Recurrent breast cancer
Invasive breast cancer that has come back months or years after treatment. It can recur in the same breast, nearby lymph nodes or in another part of the body.
-
Male breast cancer
Most male breast cancers are invasive ductal carcinomas. Fewer than 1 percent of all breast cancers are diagnosed in men.
-
Paget disease of the breast
A rare form of breast cancer where cancer cells collect in or around the nipple. It causes eczema-like changes to the skin of the nipple and the areola. It's usually a sign of breast cancer in the tissue behind the nipple.
Non-invasive breast cancer – also called precancer or in situ breast cancer. The breast cancer has not spread beyond the breast tissue where it started.
-
Ductal carcinoma in situ (DCIS)
This is non-invasive breast cancer that has not spread outside the milk ducts. DCIS isn’t life threatening but is considered a precursor to invasive breast cancer and increases the risk of developing an invasive breast cancer.
-
Lobular carcinoma in situ (LCIS)
This is non-invasive breast cancer that has not spread outside the lobules where it started. Despite its name, LCIS is a benign breast condition and is not a true breast cancer.
Know the sources
Know the sources
Launched in 2014, Know Your Lemons provides cheeky, astute visual images and information to help women identify symptoms of breast cancer and manage their disease.
Young Survival Coalition is a resource dedicated to providing community, addressing the unique needs, amplifying the voices and improving the quality of life of young adults affected by breast cancer.
Founded in 2001, Rethink Breast Cancer (RBC) works to empower young people worldwide who are concerned about and affected by breast cancer. The organization aims to provide support, education, and advocacy programs and dispel myths around breast cancer as an older woman’s disease.
Clinical trials
- The Dana Farber Cancer Institute – an aggregated list of clinical studies dedicated to understanding the causes and impact of breast cancer on young adults.
- The Impact of Organised Screening Programs on Breast Cancer Stage at Diagnosis for Canadian Women Aged 40–49 and 50–59
- Mammographic Density and the Risk and Detection of Breast Cancer
- Reducing the burden of Breast cancer in Young women (RUBY) Study
- A Study to Identify Breast Cancer (IDBC) - study to validate the Syantra DX™ Breast Cancer methodology and biomarker panel using prospective samples
Citations
- Breast Cancer Statistics 2019, CA Cancer J Clin 2019;69:438–451
- What do we mean when we refer to young women? In relation to breast cancer, young women generally refers to women who are pre-menopausal. Young women can have distinct challenges from women who are post-menopausal at the time of diagnosis.
- Nasim et al., Breast cancer incidence and behavior in younger patients: a study from the Surveillance, Epidemiology and End Results database, World J Oncol, 2020 Jun;11(3):88-97. Narod, S.A., Breast cancer in young women, Nat. Rev. Clin. Oncol. 9, 460-470 (2012).
- American Cancer Society. Key Statistics for Breast Cancer.
www.cancer.org/cancer/breast-cancer/about/how-common-is-breast-cancer - Canadian Partnership Against Cancer. Breast Cancer Screening in Canada: Environmental Scan. Toronto, ON: Canadian Partnership Against Cancer; 2018.
- https://screeningforlife.ca/breast/breast-cancer/#risk_factors_things_you_can%E2%80%99t
- Shoemaker et al., Differences in breast cancer incidence among young women aged 20-49 years by stage and tumor characteristics, age, race, and ethnicity, 2004-2013, Breast Cancer Res Treat., 169, 595-606, 2018.
- Hollingsworth, A., Redefining the sensitivity of screening mammography: A review, The American Journal of Surgery 218 (2019) 411e418
- https://actt.albertadoctors.org/CPGs/Lists/CPGDocumentList/Breast-Cancer-Algorithm.pdf. Canadian Partnership Against Cancer. Breast Cancer Screening in Canada: Environmental Scan. Toronto, ON, 2018.
2023 | Syantra Inc. | 1-877-331-0516
We value your privacy.
Read about it here
Website and branding by:
IVY Design Inc.
We